Coronavirus and Acute Lung Injury
SARS-CoV-2 (COVID-19)
Hospital
Admission and monitoring
Labs
Initial CBC, CMP, PT/PTT, d-dimer, ferritin, CRP, LDH, CPK, rapid influenza
If not previously documented: HBsAg, HCV Ab, HIV antigen/antibody (concomitant infection increases clinical risk)
Daily CBC, CMP, d-dimer (if elevated at admission), PT/INR (if elevated at admission)
CXR at admission and following unexpected changes in respiratory status
Treatment
Continue any ACE, ARB, statin unless otherwise contraindicated
Convert any nebulized medications to metered dose inhaler
Hypoxemia: Supplemental O2 to maintain SPO2 90-96%, remdesivir (see severe disease below)
Acetaminophen PRN fever
DVT prophylaxis
Severe disease/clinical deterioration
Labs
Severe features: WBC < 800/microL, d-dimer > 1000 ng/mL, ferritin > 500 mcg/L, CRP > 100 mg/L, LDH > 245 U/L, CPK > 2x ULN, troponin > 2x ULN
LDH q24h, troponin q48h
Hypoxemia requiring supplemental O2
Dexamethasone 6 mg (PO or IV) qd x 10 days or until discharge (NNT to prevent 1 death = 36)
Remdesivir 200 mg IV day 1 followed by 100 mg IV qd until discharge (maximum duration 10 days)
Indications for intubation: Rapid progression over a few hours, failure to improve despite HFNC >50 L/min and FiO2 >0.6, hypercapnia despite BiPap, hemodynamic instability, multiorgan failure (see undifferentiated shock)
Suspected superimposed bacterial infection due to sudden deterioration/CXR suggesting progressive pneumonia
Procalcitonin is often elevated in COVID and may not indicated bacterial PNA
Blood cultures x 2, sputum cultures
Appropriate pneumonia treatment
Elevated troponin or evidence of cardiomyopathy (e.g. persistent hypotension): Echocardiogram
Post-COVID Syndromes
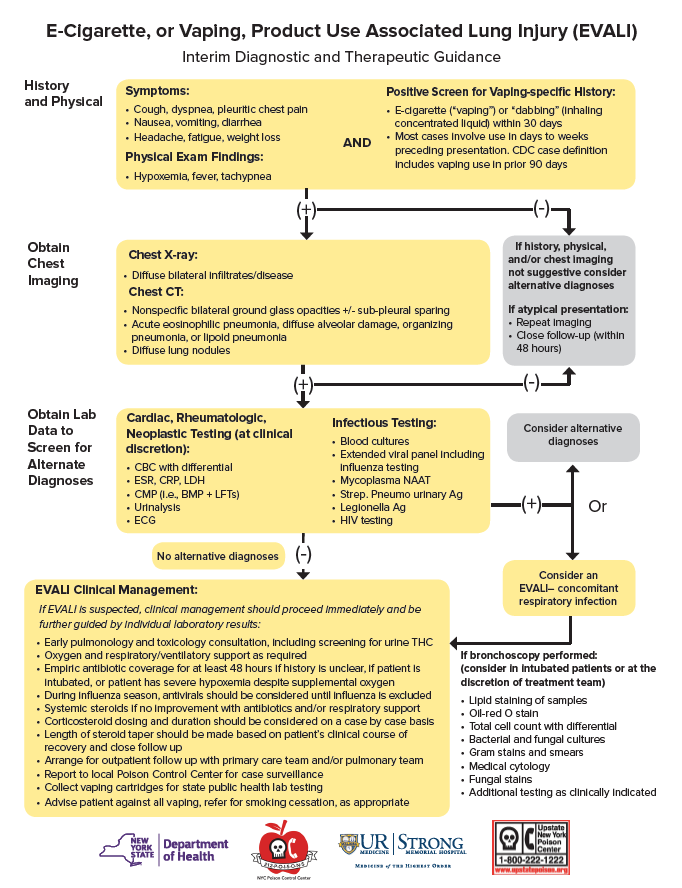
E-Cigarette and Vaping Associated Lung Injury (EVALI)
Acute Respiratory Distress Syndrome
More information coming soon…
Transfusion Associated Lung Injury (TRALI)
More information coming soon…