Health Maintenance
Plan
All Patients
[Age] year old [gender] presents for HME
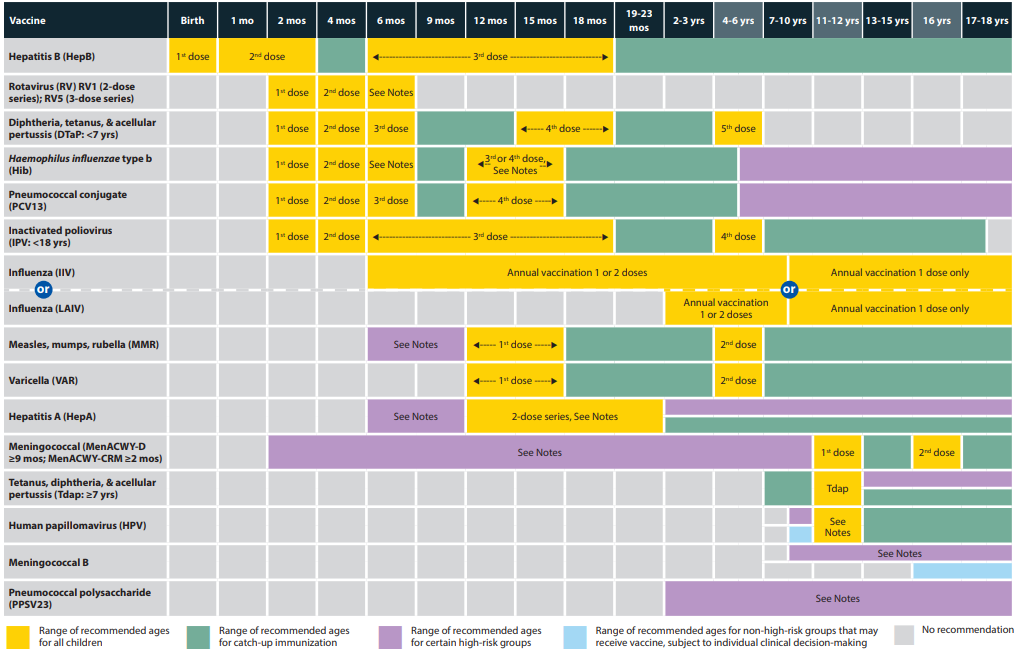
#Vaccination (≥ 22 y/o)
Influenza season: Administer influenza vaccine
Most recent TDaP ≥ 10 years ago: Administer TD booster
≤ 26 y/o with no history of HPV immunization and not currently pregnant: Administer 1st dose HPV vaccine and follow up in 2 to 6 months for the 2nd, 3rd dose
≥ 50 y/o with no history of HZV immunization, immunocompromised state: Administer 1st dose Shingrix (RZV) vaccine, follow up in 2 to 6 months for 2nd dose
≥ 65 y/o: Administer 1 dose Pneumococcal polysaccharide vaccine (PPSV23)
Born after 1980 with no varicella immunity and not currently pregnant: Administer 1st dose varicella vaccine, follow up in 4 to 8 weeks for 2nd dose
Born after 1957 and not currently pregnant: Ensure patient has received at least one MMR vaccine
Chronic disease or other risk factors (any age)
#Depression screen: Perform PHQ-2
#Alcohol use: Counsel about appropriate intake limits for age and sex
#Tobacco use: Perform tobacco cessation counseling lasting ≥ 3 minutes
Smoking cessation pharmacotherapy (select one)
Start nicotine patch
No history of mental illness, suicidal ideation: Start varenicline 1 week before quit date (0.5 mg qd days 1-11, 1 mg qd days 12-42). Follow-up in 12 weeks to review continuation for an additional 12 weeks.
Start bupropion SR 150 mg qd days 1-3 then increase to 150 mg BID
55-80 y/o with ≥ 30 pk/yr history, smoked within past 15 years, and candidate for lung surgery: Refer for yearly low-dose CT
65-75 y/o male with who has ever smoked: Refer for one-time AAA U/S screening
#STI/ID
Age 15-65 years: Screen for HIV
Engaged in high-risk sexual behaviors: Screen for hepatitis B, syphilis and offer preexposure prophylaxis (PrEP) therapy
At increased risk for TB: Place PPD and follow up for read in 48-72 hours
#Obesity (BMI > 30 kg/m2): Perform brief counseling about diet and exercise. Refer for further behavioral/dietary counseling.
#HTN: Repeat BP in office >140/>90. Trial of lifestyle modification and follow-up in 1-3 months. If BP still elevated, start antihypertensive therapy (select one):
Amlodipine 5 mg qd
Chlorthalidone 25 mg qd and obtain BMP in 2 weeks
History of HF, left ventricular hypertrophy, MI, DM, ADPKD and no history of CKD: Start lisinopril-HCTZ 10-12.5mg qd and obtain BMP in 2 weeks
#Skin cancer prevention in fair-skin patient ≤ 24 y/o: Counsel about UV radiation and sunscreen use
Age ≥ 40 years
#DM screening (40-70 y/o with BMI > 30 kg/m2): Obtain HbA1c
#Lipid screening (40-75 y/o): Obtain lipid panel and repeat every 3 years if not already taking a high-intensity statin
#Statin therapy: 40-75 y/o with CVD risk factor (MI/stent/angina, CVA, DM, PAD, HTN, smoking) and/or ASCVD risk > 10%. Start statin therapy.
Age ≥ 50 years
#Aspirin therapy: 50-59 y/o with life expectancy > 10 years, willing to take aspirin for > 10 years, and ASCVD > 10%. No history of GI bleed, coagulopathy, or other bleeding risk. Start aspirin 81mg qd for prevention of CV disease, colon cancer.
#Colon cancer screen (50-75 y/o): Colorectal CA screening with FIT every 1 year or colonoscopy every 10 years.
#Hepatitis C Screen: Born between 1945-1965 with no previous h/o Hep C screening. Obtain one time hepatitis C screen.
#Age > 65 years and at increased risk for falls: Recommend exercise interventions for fall prevention.
Women’s Health
#Age 18-65 years
≤ 24 y/o and sexually active: Screen for chlamydia/gonorrhea infection
Capable of pregnancy: Start 0.4 mg folic acid daily
Domestic violence screen: Patient feels safe at home
#Cervical cancer screen
#Breast cancer screen
Age ≥ 35 years with family h/o breast, ovarian, tubal, or peritoneal cancer: Administer screening tool, e.g. Pedigree Assessment Tool to assess need for genetic counseling, BRCA screening
Age >50 years: Mammogram every 2 years
No prior breast CA diagnosis and at increased risk: Administer screening tool to assess benefit/risk of tamoxifen/raloxifene therapy. If screening positive and patient willing to undergo treatment, consider tamoxifen 20mg vs. raloxifene 60 mg x 5 years
#Osteoporosis Screen: Age ≥ 65 years and/or positive osteoporosis risk assessment tool. Obtain DEXA scan.
Notes
Screening per USPSTF A and B recommendations
Vaccines
Second doses of HZV (Shingrix) and VZV may be administered 2 months following the first dose
Adults born before 1957 are consider MMR immune with the exception of health care workers
Vaccines are often referred to by trade names
Definition of ever smoke is 100 cigarettes in a lifetime (see AAA screening for males age 65-75 years)
Examples of high risk sexual behaviors include
There are no clear guidelines concerning repeat lipid screening. Repeating every 3 years is a conservative recommendation per expert opinion.