Dermatology

Dermatology
Adolescent F presents with gradual appearance of comedones, papules/pustules, and nodules on face. Denies use of androgens/steroids, isoniazid, lithium, phenytoin (Dilantin). Non-inflammatory nodules, inflamed comedones, and nodules noted on face, back.
Treatment
Stage 1
Noninflamed (blackheads and whiteheads)
Apply topical tretinoin 0.025% gel to acne lesions daily at bedtime
Stage 2
Inflamed comedones with few papules/pustules (pimples)
Apply benzoyl peroxide 10% gel sparingly twice daily; reduce frequency to once daily if excessive skin dryness occurs
Stage 3
Nodular lesions
Apply thin film of topical erythromycin 2.0% gel BID
Stage 4 refractory nodular/scarring acne: Start oral isotretinoin 1.0 mg/kg/day x 20 weeks and require pt
Enroll in iPLEDGE program
Obtain CBC, CMP, and fasting lipid panel
Obtain negative pregnancy test before starting medication and before each refill
Use two forms of birth control before engaging in sexually activity
Female: Consider combined oral contraceptives at any stage for improved acne control
Refractory acne: Refer to dermatology
Counseling
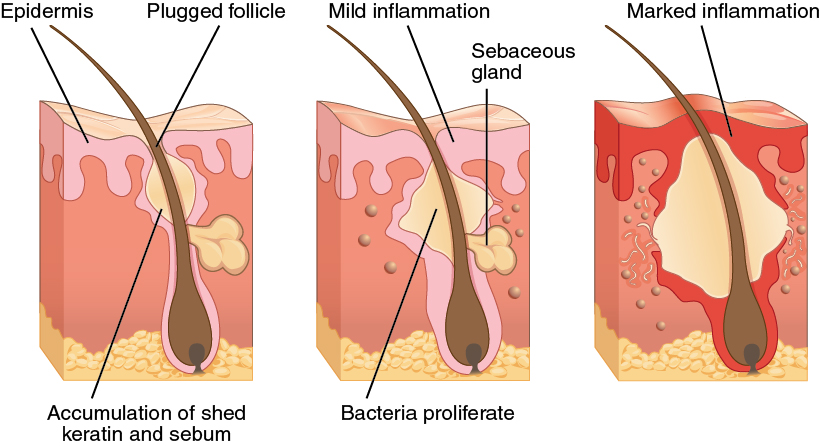
Pt counseled that acne is caused by bacterial infection with P. acnes
Pt informed that a minimum of 6-8 weeks is required to assess effectiveness of any one therapy
Pt advised that laser and light therapies are ineffective
Pt counseled that failure to comply with treatment may lead to continue acne and/or scarring

Rule out drug induced acne which may be caused by androgens/steroids, isoniazid, lithium, phenytoin (Dilantin)
Tretinoin = vitamin A derivative
Benzoyl peroxide (topical antiseptic)
Reduces risk for bacterial resistance when used with antibiotics
Pt may stop daily use once symptoms are controlled
Isotretinoin
Provider and pharmacy must be registered with iPLEDGE
Results
Long term remission in 40% of patients
40% of patients controlled with topical therapy after course
20% require re-treatment with isotretinoin
6 month old female with no history of immunodeficiency disorders presents with chronic greasy scaling of the scalp. Lesions to not appear to irritate infant. Yellow-brown scaling on well-demarcated erythematous plaques covering scalp on exam.
Recommend physical removal of plaques and regular hair washing
Parents advised that condition generally resolves by 1 year of age
55 year old male with history of parkinsonism and HIV presents with chronic greasy scaling of the skin. Reports mild, intermittent pruritus in affected regions. Patient has noted dermatitis improvement since starting L-dopa therapy and antiretrovirals. Greasy yellow scales present on scalp, central face, chest, ear canal, and groin.

Facial seborrheic dermatiti. By Roymishali.
Head: Start ketoconazole 2% shampoo
Apply twice weekly and leave in place for 5 to 10 minutes before rinsing
Continue for 4 weeks and then transition to once weekly use to prevent relapse
Face/Body
Apply ketoconazole 2% cream BID to affected areas x 4 weeks and then stop for 4 weeks before restarting
Corticosteroid: Apply BID x 2 weeks and then discontinue for 2 weeks before restarting
Face: Hydrocortisone cream 2.5% (Group 7)
Body: Triamcinolone acetonide cream 0.1%
Seborrhea refractory to initial treatment and no history of elevated AST, ALT: Start itraconazole 200 mg qd x 7 days
Notes
Pathophysiology (suspected): Abnormal immune response to Malassezia yeast
Epidemiology
Most common in children < 1 year and adults > 40 years old
Risk factors in adults: Parkinsonism, untreated HIV
Most commonly occurs in regions with high concentrations of sebaceous glands, e.g. head/face
Differential in adults includes
Common: Psoriasis, rosacea, tinea capitis, tinea corporis, tinea versicolor
Less common: Lupus erythematosus, pemphigus foliaceus, secondary syphilis
Pt with h/o atopy presents with pruritic, erythematous, and scaly skin lesions.
Start topical steroids; agent choice pending location and severity of irritation
Group 7: Hydrocortisone cream 2.5%
Group 6: Triamcinolone acetonide cream 0.025%
Group 5: Triamcinolone acetonide ointment 0.025%
Group 4: Triamcinolone acetonide cream 0.1%
Group 3: Triamcinolone acetonide cream 0.5%
Group 2: Clobetasol propionate cream 0.025%
Group 1: Clobetasol propionate cream 0.05% (group 1)
Refractory eczema in pt age 2 + years: Start pimecrolimus 1% cream
Counseling
Educated about skin atrophy risk with topical corticosteroid use
Regular, liberal use of emollients recommended
Note: Group 1 is the most potent and group 7 is the least potent
35 y/o M with a h/o HTN, DM, and tobacco/alcohol abuse disorder presents with pruritic skin scaling. Reports recent skin trauma in the most heavily affected areas. Family history includes psoriasis. BMI > 35 kg/m^2. Physical exam reveals sharply defined, erythematous plaques overlying course scales present on the scalp, ear, extensor surface of elbows, knees, and gluteal cleft. Plaque size ranges from 1 to 10 cm with positive Auspitz sign.

Plaque psoriasis affecting extensor surface of arm. Image by MediaJet.
Initial treatment
Start topical steroids
Apply two weeks and then discontinue for two weeks
Patient may continue two week cycle of use and discontinuation if symptoms recur
Scalp psoriasis
Apply 3% coal tar shampoo (e.g. MG 217) to wet scalp and leave in place for 5 minutes before rinsing
Continue daily use until symptoms resolve
Refractory disease
Continued symptoms despite steroid use: Add topical calcitriol twice daily to affected areas (maximum weekly dose 200 g)
Consider skin biopsy versus dermatology referral
Notes
Epidemiology
Obesity, tobacco, and alcohol use are risk factors for psoriasis
HTN and DM are often comorbid with psoriasis
Psoriasis is an autoimmune condition and may be more prevalent in patients with other forms of autoimmune disease
Presentation
The vignette describes the most common form of psoriasis, chronic plaque psoriasis
Koebner phenomenon: Development of skin lesions such as psoriasis following skin trauma
Auspitz sign: Pinpoint bleeding when overlying scale is removed
Treatment
Topical calcitriol: Vitamin D analog that can be used continuously unlike topical steroids
Tazarotene: Vitamin A analog also commonly used in psoriasis treatment
Severe disease may be treated with calcineurin inhibitors (e.g. tacrolimus) or biologic agents
More information available through the National Psoriasis Foundation
Pt with h/o smoking, metabolic syndrome, poor hygiene presents with solitary inflamed nodules in intertriginous region. Previous complications have included abscesses and formation of sinus tracts. Inflamed skin nodules tender to palpation surrounded by open comedones and scarring.
Treatment per Hurley classification
Hurley I (mild disease): Start topical clindamycin; intralesional steroids/oral antibiotics for flares
Hurley II (nodules, sinus tracts, scaring present): Start doxycycline
Hurley III (extensive sinus tracts)
Start acitretin (oral retinoids) and consider adalimumab (Humira) therapy
Refer to dermatology
Schedule for definitive treatment with wide surgical excision
Acutely inflamed nodule/sinus tract: Perform punch debridement for small nodules, unroofing for larger tracts
Chronic/extensive disease: Refer pt for wide excision of lesions
Patient counseled to stop smoking and lose weight to decrease disease severity and improve treatment response
Conditions sometimes associated with hidradenitis: Arthritis, Crohn disease, DM, metabolic syndrome, PCOS, pyoderma gangrenosum, Trisomy 21
Surgical treatment options include punch debridement, unroofing, skin sparing excision with electrosurgical peeling, and wide excision
40 y/o African American male with h/o peripheral arterial disease, ESRD requiring dialysis, DM with peripheral neuropathy, immunocompromised state, alcohol abuse presents with acute onset painful lower extremity redness and swelling. Reports recent hot tub use, athletic activity, and trauma at infection site. ROS positive for anorexia, vomiting. Fever, tachycardia, obesity, lymphedema, lymphedema, intravascular port on exam. Skin infection site reveals skin break surrounded by erythema, warmth, edema, induration, and tenderness to palpation. No bullous lesions, crepitus noted.
Systemic s/sx symptoms of infectious spread (anorexia, vomiting, abnormal vitals) in an immunocompromised patient despite initial oral antibiotics: Admit for inpatient management
Labs
Obtain CBC, CMP, CRP
S/sx of systemic involvement: Obtain blood cultures
Immunocompromised state and/or sepsis/lymphangitis on exam: Obtain wound cultures
Adult patient: Wound ultrasound not indicated
Antibiotic coverage
Uncomplicated, i.e. erythema/warmth/edema at site but no concerning risk factors or indications for hospitalization
Non-purulent: Cephalexin (Keflex) 500 mg 4x daily
Purulent infection concerning for MRSA: Doxycycline 100 mg BID
Hospitalized
Non-purulent: Ceftriaxone 1g IV qd
Purulent infection concerning for MRSA: Vancomycin 15 mg/kg q8h, maximum dose 2g; obtain trough before 4th dose with goal 10-15 if not septic

Non-purulent cellulitis of the left leg.

Cellulitis with purulent appearance.
Epidemiology
Most common in patient age 18-44 years with a male and African American predominance
75% of all community cellulitis is due to beta-hemolytic streptococcus
Group includes S. pyogenes, S. agalactiae
Consider adding cephalexin to doxycycline for improved strep coverage
Vancomycin provides good coverage for strep and MRSA
60% of ED cases initially presenting to ED are due to MRSA
Risk factors for infection
Sites of entry
Skin breaks (inspect between patients toes)
Sites of injury/trauma
Medical devices including IV drug use
Prolonged stays in medical facility
Medical history (see PMH in first line of vignette)
Immunocompromised state includes nutritional deficiency, asplenia, HIV, and medication use (DMARD, chemotherapy, antiretroviral)
Conditions that create infection nidus, e.g. obesity, lymphedema
Profession: Health care professional, military personnel
Activities: Sports participation, swimming (e.g. hot tub use)
Management
Consider and rule out potential emergencies, e.g. gangrene, necrotizing fasciitis as indicated by pain out of proportion, bullae, crepitus
Labs/Imaging
Blood cultures rarely change management in immunocompetent patients
In adolescents, ultrasound improves diagnostic accuracy
Reasons for hospitalization
Cannot tolerate PO antibiotics
Continued infection despite outpatient antibiotics
Complicated initial presentation including s/sx infectious spread (fever, tachycardia, anorexia, vomiting)

IDSA Flowchart for Antibiotic Selection. Downloaded from https://academic.oup.com/cid/article-abstract/59/2/e10/2895845 by guest on 18 January 2019.
Pediatric pt presents with multiple hyperpigmented macules and patches. Some lesions have been present since birth while others developed in childhood. Family h/o 1st degree relative with neurofibromatosis type 1. Exam reveals axillary/groin freckling, two cutaneous neurofibromas, and multiple hyperpigmented macules/patches with discrete borders measuring 0.2 to 30 cm in diameter.

A cafe au lait birthmark on the left cheek of a patient with a U.S. dime used to indicate scale.
Refer to ophthalmology to evaluate for iris hamartomas (Lisch nodules) and optic gliomas
Refer for genetic consultation
Pt advised that surgical or laser ablation of cafe au lait spots is only indicated for cosmetic purposes

Adult patient with multiple small cutaneous neurofibromas and a café au lait spot (bottom of photo, to the right of center).
Cafe au lait spots can be benign or associated with neurofibromatosis
If a patient does not meet NIH neurofibromatosis criteria, the macule is benign
NIH criteria for neurofibromatosis requires the presence of two or more of the following:
Six or more café au lait macules/patches larger than 5 mm in greatest diameter in prepubertal persons and larger than 15 mm in greatest diameter in postpubertal persons
Freckling in the axillary or inguinal region
Two or more neurofibromas of any type or one plexiform neurofibroma
Optic glioma
Two or more Lisch nodules (iris hamartomas)
A distinctive osseous lesion such as sphenoid dysplasia or thinning of long bone cortex with or without pseudoarthrosis
A first-degree relative (i.e., parent, sibling, child) with neurofibromatosis type 1 by the above criteria

Superficial spreading melanoma arising from a dysplastic nevus.
50 y/o white M with h/o extensive UV exposure and moles/dysplastic nevi presents with a hyperpigmented, macular skin lesion on trunk. Lesion has recently increased in shape, size, and appearance. Positive family h/o cutaneous melanoma. Flat/palpable hyperpigmented macule with asymmetric/irregular borders, color variation, and diameter > 6mm on exam.
Dermoscopy reveals asymmetric color distribution and starburst pattern.
Scoop shave biopsy positive for melanoma
Refer to surgery for melanoma resection with margins per Breslow depth
Lesion depth greater than 1.0 mm; refer for sentinel lymph node biopsy to determine stage/prognosis
Epidemiology
3 to 5% of all skin cancers
Responsible for 75% of skin cancer deaths
At-risk populations
Most cases occur in white males > 65 years
Most common cancer in women age 25-29 years
Subtypes include superficial spreading, nodular, lentigo, amelanotic, acral-lentiginous, subungual
Superficial spreading
Most common subtype (70% of melanomas)
Occur between ages 30-50 years
Typically located on trunk in men and legs in women
Nodular
Second most common subtype (10-15%)
Generally occur in men on the trunk, head, or neck
Diagnosis
ABCDE: Asymmetry, border irregularities, color variation, diameter, and evolution
Dermatoscope
Device used to magnify lesion under polarized light
Increases diagnostic accuracy by 10-27%
Biopsy: Scoop shave or punch biopsy can be performed
Breslow depth: Histopathologic depth of lesion used to determine prognosis and surgical margins
Surgical margins
Per Breslow depth
In situ = 5 mm margins
2.0 mm depth or less = 1 cm margins
> 2.0 mm depth = 2 cm margins
Narrow (1-2 cm) vs. wide surgical margins (3-5 cm) do not impact survival
Pt > 50 y/o with h/o smoking, significant UV-B exposure presents with suspicious appearing papule. Reports frequent tanning bed use in adolescence. Exam reveals pearly white, dome-shaped papule with prominent telangiectatic surface vessels on nose.

BCC Nodular type. Red, waxy nodule on the tip of the nose. Visible telangiectasias over the surface.
Shave biopsy performed and sent for histopathology; positive for BCC
Treatment
Nodular or superficial subtype < 3 mm in depth; treat with cryotherapy
Tumor diameter < 2 cm and not located on H region of face; refer for standard surgical excision
Refer for Mohs micrographic surgery for tumors
Located on H region of face
> 2 cm in diameter
With invasive histologic subtype and/or high risk of recurrence
Pt counseled about risk of recurrence and importance of monitoring for future lesions
Schedule f/u yearly s/p tumor removal
Epidemiology
BCCs comprise 80% of non-melanotic skin cancers and rarely metastasize
Tanning bed use is associated with 1.5-fold increase in BCC risk
Histologic subtypes
Nodular (21%)
Superficial (17% and may resemble eczema or psoriasis)
Invasive subtypes
Micronodular (15%)
Infiltrative (7%)
Morpheaform (1%)
Presentation
85% occur on patients face with 25-30% occurring on the nose
Pigmented BCC may be confused with melanoma
Diagnosis: Shave or 2-4 mm punch biopsy may be performed
Risk of recurrence
Determined by lesion location, size, border definition, and status as primary or recurrent
Overall: 35% at 3 years and 50% at 5 years