Respiratory
Respiratory

Asthma Severity and Associated Therapy. Fluticasone or a similar inhaled corticosteroid should be started before medications in gray are added. For more information see Obstructive Lung Disease Medications, Asthma Quick Care Reference, and the NIH Expert Panel Report Guidelines (2007).
More information coming soon. See information about common asthma myths to discuss when counseling patients.

Patient with history of asthma, atopic dermatitis, seasonal allergies, and smoking presents with acute on chronic dyspnea. Exacerbations typically display a seasonal pattern. Reports rhinorrhea as well as recent exposure to cleaning product vaports, second-hand smoke, wood burning stove, pets, cockroaches, and mold. Medications include NSAIDs, beta-blockers, and ACE inhibitors. Tachypnea, retractions, and inspiratory/expiratory wheezes on exam. Cannot count to three in one breath.
More information coming soon. See information about common asthma myths to discuss when counseling patients.
Pediatric patient with h/o asthma, atopic dermatitis, and seasonal allergies presents with acute on chronic dyspnea. Exacerbations typically display a seasonal pattern. Parent reports recent rhinorrhea and NSAID administration. Cleaning product vaports, second-hand smoke, wood burning stove, pets, cockroaches, and mold present in home. Tachypnea, head bobbing, nasal flaring, subcostal/intercostal/substernal/supraclavicular retractions, and inspiratory/expiratory wheezes on exam. Cannot count to three in one breath.

Pediatric Asthma Severity Score (PASS) range 0-6 for evaluation of acute, outpatient asthma. Source: Children’s Hospital of Philadelphia Asthma Clinical Pathway - Primary Care.
Outpatient
Obtain peak flow and compare to baseline
Initial respiratory score: If ≤ 5, proceed with treatment in office. Otherwise, refer family to the nearest emergency department.
Administer albuterol MDI x 8 puffs
Administer dexamethasone 0.6 mg/kg x 1 (maximum 16 mg)
Review asthma action plan with parent and child
Observe for 1 hour
Reassess respiratory score after 1 hour
If ≤ 4, return home with appropriate increase in therapy (see Asthma Severity and Associated Therapy above) and follow up in 2 weeks
If > 4, refer family to the nearest emergency department
Emergency Department
All patients
Start supplemental oxygen to maintain SPO2 > 90%
Start albuterol MDI or nebulizer (see below)
Administer dexamethasone 0.6 mg/kg x 1 (maximum 16 mg)
Respiratory score 6-9: Add ipratropium nebulizer
Respiratory score 10-12: Add magnesium sulfate
Reassess at hours 2, 3, and 4 and adjust therapy and/or admit as indicated below

Asthma Pediatric Respiratory Score for evaluation of inpatient pediatric asthma exacerbations. Source: Seattle Children’s Hospital.
Asthma is more common in patients with a history of atopy, e.g. eczema and seasonal allergies
Seasonal exacerbations may occur during the spring (pollen/weather change), summer (humidity), fall (weather change), and/or winter (cold)
Medications that may worsen asthma include NSAIDs, beta-blockers, and ACE inhibitors
Asthma exacerbation triggers commonly include
Respiratory illness
Allergen/environmental exposures
Smoke/vapors, e.g. smokin, second-hand smoke, wood burning stoves, cleaning products
Animals, e.g. household pets and cockroaches
Mold in houses, including air conditioning units
See Asthma Management Pathway from Seattle Children’s Hospital (below) for management and dosing information.

Information about common asthma myths to review when counseling patients. Source: Chest Foundation and Asthma and Allergy Network.

Asthma ED Pathway. Source: Seattle Children’s Hospital.

Asthma Inpatient Pathway. Source: Seattle Children’s Hospital.
Pt > 45 y/o with 40+ pack/year smoking history, chronic air pollution/occupational dust exposure presents with dyspnea. Reports chronic cough, wheezing. Family history includes alpha-1 antitrypsin deficiency. Maximal laryngeal height < 4 cm, diminished breath sounds, wheezing on exam.
Administer COPD Assessment Test (CAT)
Refer for spirometry: Evaluate for FEV1/FVC < 0.7, peak flow < 350 L/min
Imaging
Previous x-ray shows lung hyperinflation with flattened hemidiaphragms
Dyspnea out of proportion to spirometry: Consider
Echocardiogram to rule out pulmonary arterial hypertension
CT angiography to rule out pulmonary embolism
Treatment
Vaccination: Administer yearly influenza vaccine
Age 19-64 years: 1 dose PPSV23
Age 65+ years: 1 dose PCV13 followed by PPSV23 in 1 year
GOLD category 1-2 (FEV1/FVC ≥ 50%) and ≤ 1 exacerbation per year
A. CAT < 10: Albuterol ER 4 mg BID (SABA)
B. CAT ≥ 10: Add tiotropium (anticholinergic) 1 puff/day
GOLD category 3-4 (FEV1/FVC < 50%) or 2+ exacerbations per year
C. CAT < 10: Albuterol ER 4 mg BID + tiotropium 1 puff/day + pulmonary rehab referral
D. CAT ≥ 10: Albuterol ER 4 mg BID + fluticasone/salmeterol 1 puff BID + pulmonary rehab referral; consider roflumilast
Resting SPO2 < 88% or PaO2 < 60 mmHg: Start supplemental oxygen and refer to pulmonology
Smoking cessation: Pt advised to stop smoking to reduce further FEV1 decline

Notes
FEV1 GOLD category
Category 1: ≥ 80%
Category 2: 50-79%
Category 3: 30-49%
Category 4: < 30%
Treatment: See Obstructive Lung Disease Medications for further details
Supplemental oxygen
Decreases mortality when indicated
The only proven therapy for COPD-related PAH
Tiotropium and salmeterol have been shown to reduce hospitalization
Avoid short acting anticholinergics in patients with cardiac disease
Fluticasone/salmeterol = corticosteroid/LABA (brand name Advair)
Roflumilast (Daliresp) = PD4 inhibitor
Pt > 45 y/o with 40+ pack/year smoking history presents with acute on chronic dyspnea. Reports recent sick contact and exposure to allergens followed by increased dyspnea, sputum volume, and sputum purulence. Acute dyspnea worse with exertion. SPO2 < 90%, diffuse wheezing bilaterally on exam.
Admit to inpatient for any of the following: Failed outpatient therapy, rapidly worsening dyspnea/hypoxia/hypoxemia, altered mental status
CBC, BMP and consider ABG
CXR to exclude pneumonia, pneumothorax, pulmonary edema, pleural effusion
Initial treatment
Duoneb (albuterol 2.5 mg/ipratropium 0.5 mg) 1 vial q4h while awake
Prednisone 50 mg x 5 days to reduce risk of symptom relapse
Home medications
Hold Spiriva (tiotropium) 1 puff qd; restart upon discharge
If CAT ≥ 10 with FEV1 < 50% or 2+ exacerbations in the past year, start Advair 1 puff BID at discharge
Titrate O2 to maintain SPO2 > 88% and consider CPAP if evidence of chronic hypercapnia
Antibiotic coverage for moderate to severe exacerbations involving increased sputum purulence
No additional risk factors: Azithromycin 500 mg x 1 day followed by 250 mg x 4 days
Concern for PNA or risk factors for poor outcome (age ≥ 65 years, ≥ 2 exacerbations/year, h/o cardiac disease): Augmentin 875 mg BID x 5 days
Pseudomonas risk factors (previous infection, frequent hospitalization, systemic glucocorticoids)
Obtain sputum gram stain and culture
Consider adding Zosyn 4.5 g IV q6h if condition deteriorates
Vaccination and smoking cessation: See section on chronic COPD management (above)
Notes
Three cardinal symptoms: Increased dyspnea, increased sputum volume, and increased sputum purulence
Pathogens associated with pneumonia risk: S. pneumoniae, H. influenza, Moraxella
Antibiotic therapy x 5-7 days during exacerbations
Only beneficial for patients who meet one of the following criteria (GOLD 2019):
Increased sputum purulence + at least one additional cardinal symptom
Moderate to severe exacerbation (meet one of the following): Accessory muscle use, RR > 30 BPM, change in mental status, PaCO2 > 50 mmHg
Require mechanical ventilation
If appropriate, may shorten recovery time and reduce risk of early relapse, treatment failure, hospitalization duration
Continuous antibiotic prophylaxis, e.g. azithromycin 250 mg MWF may reduce exacerbation frequency, but is not effective beyond 1 year
Pt > 50 y/o M with h/o obesity, HTN, CAD, cardiac arrhythmias, depression presents with partner complaints of loud snoring/gasping during sleep. Reports morning headache, daytime sleepiness. Currently being treated for HTN. BMI > 35 kg/m^2, neck circumference > 40 cm on exam.
STOP-BANG = 8
Refer for sleep study
Pt advised to lose weight with goal of reducing BMI to < 35 kg/m^2
Sleep study positive
Treatment with CPAP vs. oral appliance
Consider placing tennis ball in sock and pinning it to back of shirt to avoid supine sleeping position
Consider referral for surgery for refractory OSA
CPAP improves daytime sleepiness, but does not reduce risk of cardiovascular events
Snoring
DDX
Upper airway resistance syndrome (UARS)
Stridor
Risk factors
increasing age
male gender
obesity (BMI >30)
craniofacial abnormalities
History
noisy breathing during sleep
apneas
choking or gasping
waking up tired
daytime somnolence
hyperactivity
behavioral problems
Initial work-up
nasal decongestant test
Epworth sleepiness score (ESS)
Also consider
snoring scale score
TFTs
growth hormone level
allergy tests
[] Do you snore loudly?
[] Do you often feel tired, fatigued, or sleeping during the daytime?
[] Has anyone observed that you stop breathing, or choke or gasp during your sleep?
[] History of HTN
[] BMI > 35
[] Age > 50 years
[] Neck circumference > 40 cm
[] Male gender
Scoring
0-2 (low risk)
3-4 (intermediate risk)
>5 (high risk)
Elderly pt with no h/o alcoholism, dysphagia, cardiopulmonary/liver/renal disease, DM, asplenia, malignancy, and immunosuppression including HIV and IV drug use presents from home with dyspnea. Reports malaise, fever/chills, productive cough, pleuritic chest pain, myalgias, and night sweats. Denies rhinorrhea, sore throat. Recently returned from a cruise. Fever, hypotension, tachycardia with increased work of breathing, pulmonary crackles, and egophony on exam.
Labs
Obtain SPO2, BMP
Obtain CBC, blood cultures upon hospitalization
Consider obtaining pneumococcal/Legionella urine antigen test and procalcitonin for risk stratification
Recent high risk sexual exposure/IV drug use: Consider testing for HIV, TB, pneumocystis pneumonia (PCP)
Imaging
Obtain EKG upon hospitalization to rule out QT prolongation
CXR showing pulmonary opacities and lobar infiltrate
Calculate CURB-65 (confusion, BUN > 19, RR > 30, BP < 90/60, age 65+) to determine need for hospitalization
Treatment
Outpatient: CURB-65 < 2
Start azithromycin 500 mg on day 1 followed by 250 mg days 2-5
Contact office if symptoms worsen or fail to improve with treatment
Hospitalized patient (CURB-65 2+) with no QTC prolongation and normal renal function:
Start ceftriaxone (CTX) 1g IV qd + azithromycin 500 mg IV qd x 5 days
Pseudomonas risk factors: Substitute piperacillin-tazobactam (Zosyn) 3.375g q6h x 7 days for CTX
MRSA risk factors: Add vancomycin 20 mg/kg/dose (max 2g) BID x 7 days
Admitted to ICU: Consider prednisone 50 mg qd x 5 days to decrease length of stay/ARDS risk
Age 65+ years: PCV13 vaccine prior to discharge and PPSV23 in 12 months
Alcoholism, dysphagia, and/or other aspiration risk factors
Outpatient: Amoxicillin-clavulanate ER 875 mg BID + azithromycin
Hospitalized: Ampicillin-sulbactam 1.5 g IV q6h + azithromycin
Notes
The vignette presentation is a severe CAP case that would require hospitalization. It is written to help you take a more complete history.
For less severe presentations and CURB-65 < 2, treat as an outpatient. A BMP is required to calculate CURB-65 and should be obtained in more severe cases.
Patient without any of the risk factors mentioned in the vignette can be treated outpatient with azithromycin (see above)
Clinical presentation
Pleuritic chest pain: Sharp stabbing/burning sensation present while inhaling (primarily) and exhaling
Fever (LR+ 2.7) and egophony (LR+ 5.3) are the most predicative physical findings
Rhinorrhea and sore throat may be present, but are more indicative of viral URI
Treatment in hospital
IV antibiotics indicated if any are present: Cognitive impairment, inability to tolerate PO, HR > 100, SPO2 < 90%, RR > 25, T > 38.4
Alternative regimen for non-ICU patient without risk factors:
Ceftriaxone 2g BID x 5 days (beta-lactam) + azithromycin 500 mg qd x 5 days (macrolide)
If QTc elevated, substitute doxycycline 100 mg BID x 5 days for azithromycin
Pneumonia requiring ICU admission: 3rd generation cephalosporin (CTX) + macrolide (azithromycin) +/- respiratory fluoroquinolone (levofloxacin, moxifloxacin)
Pneumonia subtypes
Aspiration pneumonia
Alcoholism and dysphagia increase risk
Require anaerobic coverage with a macrolide (e.g. azithromycin), fluoroquinolone (e.g. levofloxacin), or doxycycline
MRSA PNA: Risk factors include components of the Schorr score (consider MRSA coverage for ≥ 7 points)
Legionella pneumonia
Risk factors include cruise ship travel
May present with diarrhea and hyponatremia
Levofloxacin covers Legionella (do not obtain a urine Legionella NAAT if using this medication)
When taking a history, the CAP vignette still applies with the exception of presenting from home
HAP definition: PNA occurring within 48 hours of admission that was not present at the time of admission
Healthcare associated pneumonia (HCAP) was not included in the 2016 IDSA guidelines
Antibiotic selection: Refer to a local antibiogram for specific resistance patterns. One will generally be available through a hospital EMR or intranet page.
Levofloxacin 750 mg x 7 days
MRSA coverage
Start if risk factors for MRSA pneumonia are present or if local methicillin resistance is > 20% or unknown
Add linezolid 600 mg IV BID x 7 days
Structural lung disease, treatment with IV antibiotics during previous 90 days, and/or need for ventilatory support: Add Ceftazadime 2 g IV q8h x 7 days to levofloxacin and linezolid coverage
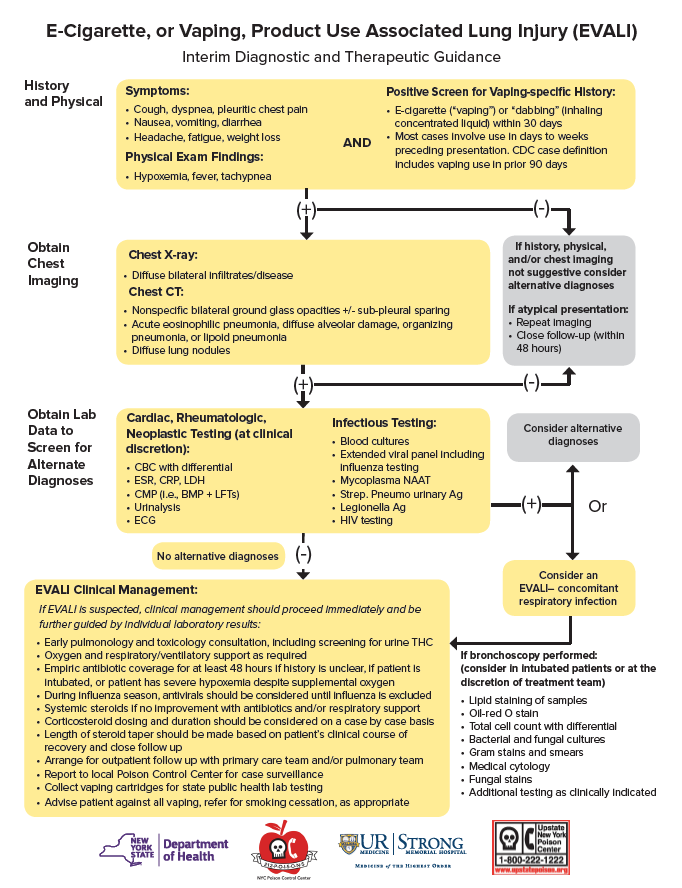
When evaluating for pneumonia, also consider acute lung injury including:
Acute Respiratory Distress Syndrome (ARDS)
E-cigarette or Vaping Product use Associated Lung Injury (EVALI)
Transfusion Associated Lung Injury (TRALI)
Hospital
Admission and monitoring
Labs
Initial CBC, CMP, PT/PTT, d-dimer, ferritin, CRP, LDH, CPK, rapid influenza
If not previously documented: HBsAg, HCV Ab, HIV antigen/antibody (concomitant infection increases clinical risk)
Daily CBC, CMP, d-dimer (if elevated at admission), PT/INR (if elevated at admission)
CXR at admission and following unexpected changes in respiratory status
Treatment
Continue any ACE, ARB, statin unless otherwise contraindicated
Convert any nebulized medications to metered dose inhaler
Hypoxemia: Supplemental O2 to maintain SPO2 90-96%, remdesivir (see severe disease below)
Acetaminophen PRN fever
DVT prophylaxis
Severe disease/clinical deterioration
Labs
Severe features: WBC < 800/microL, d-dimer > 1000 ng/mL, ferritin > 500 mcg/L, CRP > 100 mg/L, LDH > 245 U/L, CPK > 2x ULN, troponin > 2x ULN
LDH q24h, troponin q48h
Hypoxemia requiring supplemental O2
Dexamethasone 6 mg (PO or IV) qd x 10 days or until discharge (NNT to prevent 1 death = 36)
Remdesivir 200 mg IV day 1 followed by 100 mg IV qd until discharge (maximum duration 10 days)
Indications for intubation: Rapid progression over a few hours, failure to improve despite HFNC >50 L/min and FiO2 >0.6, hypercapnia despite BiPap, hemodynamic instability, multiorgan failure (see undifferentiated shock)
Suspected superimposed bacterial infection due to sudden deterioration/CXR suggesting progressive pneumonia
Procalcitonin is often elevated in COVID and may not indicated bacterial PNA
Blood cultures x 2, sputum cultures
Appropriate pneumonia treatment
Elevated troponin or evidence of cardiomyopathy (e.g. persistent hypotension): Echocardiogram
Post-COVID Syndromes
More information coming soon…
More information coming soon…
40 y/o patient with h/o asthma, COPD, and workplace exposure to lung irritants presents with cough symptoms lasting < 3 weeks. Reports recent upper respiratory illness. Non-productive cough on exam.
Symptom management by age
> 1 y/o: Administer 1 teaspoon honey q6h PRN
> 4 y/o: Consider dextromethorphan for cough suppression
> 12 y/o and not pregnant: Consider decongestants (e.g. pseudoephedrine) for relief of nasal congestion
Counseling
Pt advised that cough is likely related to recent viral illness
Pt advised to avoid occupational/environmental exposure
Pt advised to follow-up if cough persists for >8 weeks
Additional risk factors
Endorses dyspnea: Consider workup for heart failure and/or obstructive airway disease
Reports hemoptysis
Obtain CXR
Age 40+ years with 30+ pack/year smoking history
CXR negative for pathology: Obtain CT
CT negative with persistent hemoptysis: Refer to pulmonology for evaluation +/- bronchoscopy
Pt with h/o smoking, COPD, HTN, upper airway cough syndrome, GERD, asthma, non-asthmatic eosinophilic bronchitis presents with cough x8 weeks. Reports vomiting, chest pain, brief syncopal episode, and difficulty sleeping. Denies fever, weight loss, hemoptysis, hoarseness, excessive dyspnea or sputum production, recurrent pneumonia. Non-productive cough on exam; LCTAB.
Obtain CXR to r/o infectious/inflammatory/malignant conditions; if negative, initiate empiric treatment
Concern for asthma-induced cough; refer for spirometry
STOP-BANG >= 5; refer for sleep study
Switch ACE to ARB
Optimize COPD treatment
Pt advised to avoid cigarette smoke, other airborne irritants
Consider gabapentin or pregabalin for persistent symptoms
Consider CT and/or referral to pulmonology if cough etiology is not identified and initial tx not effective
Common etiologies
Upper airway cough syndrome (post-nasal drip)
Asthma-induced cough
GERD-induced cough
ACE-inhibitor induced
Less common etiologies
OSA
COPD
Sarcoidosis
Pt from Asia with h/o DM, HIV, bariatric surgery, solid organ transplant, homelessness, and incarceration presents for health maintenance exam. Works in the healthcare industry and reports ongoing substance abuse including smoking, injection drug use. Weight <90% of ideal body weight on exam.
Screening
No h/o BCG vaccine and reliable for follow-up: Mantoux tuberculin skin test (PPD) positive
H/o BCG vaccine or unlikely to return for PPD check: Interferon-gamma release assay (QuantiFERON-TB Gold) positive
Obtain CXR to rule out fibrotic changes, active disease
Treatment
Offer once-weekly isoniazid 15 mg/kg (max dose 900 mg) and rifampin (weight-based dosing guidelines) x 12 weeks
If evidence of active disease on CXR, transition to active disease regimen
Prophylax close contacts with isoniazid 15 mg/kg (max dose 300 mg) qd x 9 months
Pt counseled about concern for progression to active disease due to risk factors including DM, immunocompromised state, continued substance abuse, and h/o bariatric surgery
Pt advised that without treatment, latent TB will convert to active disease in 10% of cases

TB screening tests include PPD and interferon-gamma release assay (QuantiFERON-TB Gold)
Positive in cases of both latent and active TB
Tuberculin skin test (sensitivity 90%, specificity 80%)
> 15 mm: Positive for all patients
> 10 mm: Positive for patients
Children < 4 years old
From regions where TB is common
Who work in setting where TB is common
IV drug users
> 5 mm: Positive for patients
Who are immunocompromised (e.g. HIV, transplant recipient, prescribe ≥ 15 mg prednisone daily, etc.
With direct exposure to active TB
With fibrotic changes on CXR
QuantiFERON-TB Gold (sensitivity 80%, specificity 99%)
Not recommended for children younger than 5 years
CDC recommends against use for confirmatory testing after positive PPD
Latent TB
Risk factors for contracting infection include living abroad, working in healthcare, institutionalization (e.g. homeless shelter, prison), and immunocompromised state (e.g. HIV, solid organ transplant)
Non-symptomatic and cannot be spread to others
CXR in latent TB may be normal or show calcified granulomas
Twelve week course of isoniazid/rifapentine is as effective as 9 month course
Pt with h/o immunocompromised state, latent TB presents with hemoptysis x3 weeks. Reports fatigue, night sweats, and chest pain exacerbated by cough. Fever, weight loss, lymphadenopathy on exam.
Labs
Positive TB nucleic acid amplification and sputum acid fast bacilli (AFB) smear
Obtain CBC, CMP; consider 4th generation HIV test
Patient HIV positive: Obtain CD4 count
Imaging
CXR shows upper-lobe nodular opacities, hilar adenopathy, and patchy consolidation likely representing pleural effusion and/or pulmonary infiltrates
Consider CT to r/o disseminated disease
Drug susceptible TB treatment
Initial intensive phase (2 months)
Rifampin 600 mg daily; pt counseled that urine may appear red due to medication
Isoniazid 300 mg daily
Pyrazinamide 1,000 mg daily
Ethambutol 800 mg daily
After intensive phase, continue rifampin 600 mg daily and isoniazid 300 mg daily for 7 months
Refer to infectious disease
Report case to local health department
Patient’s social circumstances may allow transmission to other community members: Admit to hospital and initiate airborne infection precautions including negative pressure room

TB prevalence per 100,000

Advanced TB with cavitary lesion in apical segment
Infection and transmission
See latent tuberculosis for risk factors associated with acquiring TB
Airborne and highly contagious
If a patient lives alone and contact with other community members can be limited, hospital admission may not be warranted
Healthcare workers should wear N95 mask
Diagnosis
Definitively made with one of the following
Positive NAA
Two positive AFB smears regardless of NAA
If definitive diagnosis cannot be made, treat based on screening test results and clinical judgement
CXR
Abnormalities generally seen in posterior upper lobes or superior lower lobes
Hilar adenopathy is only observed in one third of cases
Treatment
In patient <55 kg lean body mass, refer to weight-based dosing
Rifampin can turn urine red, but the pt may not notice because ethambutol can cause loss of color vision
History
Presenting symptoms (sudden onset)
PE: Dyspnea, cough, hemoptysis, chest pain
DVT: Unilateral leg swelling/edema, calf pain
OR > 10 if within previous 3 months: Hip/leg fracture, spinal cord injury, cesarean section or surgery requiring general anesthesia,
OR 2-9: Pregnancy, estrogen therapy, central venous line, arthroscopic knee surgery
OR < 2: Immobilization (bedrest) due to illness/injury for 3+ days, prolonged travel in motor vehicle, varicose veins
Persistent risk factors (OR 2-9): Morbid obesity, heart failure, inherited thrombophilia, active cancer within previous 6 months +/- chemotherapy
Physical exam
Vitals (PE): Heart rate > 100 BPM, tachypnea, hypoxemia
DVT: Unilateral calf redness, warmth, swelling/edema, tenderness
Initial diagnostics
CBC, BMP
EKG: Precordial T-wave inversion, RBBB, S1-Q3-T3 suggesting PE
Less than 2: Calculate PERC and if ≥ 1, obtain d-dimer to rule out PE
Greater than or equal to 2:
Obtain lower extremity DVT ultrasound
No history of pulmonary HTN, heart failure: CT-angiography if lower extremity DVT is negative
Persistent shock including hypotension: Consider thrombolysis
Platelets > 70,000 with low hemorrhage risk and no limb ischemia, liver disease, ESRD, concerns for follow up:
Anticoagulation regimens
No morbid obesity and no current pregnancy/malignancy with weight > 60 kg and Cr < 1.5: Apixaban 10 mg BID x 7 days followed by 5 mg BID
Elevated bleeding risk: Start concomitant LMWH/warfarin x 5 days. Continue warfarin and titrate to INR 2-3.
Hemodynamically unstable with high bleeding risk, renal insufficiency, and/or morbid obesity: Start unfractionated heparin
First event
Provoked with immediately reversible risk factor: 3 months
Provoked with persistent risk factor (e.g. immobility, pregnancy): 3 months and consider extending to up to 12 months
Unprovoked and not a candidate for indefinite anticoagulation: 3 months
Repeat event: Initiate indefinite anticoagulation
IVC filter: Consider for patients who are not candidates for anticoagulation or fail anticoagulation
Counseling: Patient informed that s/he may develop post-thrombotic syndrome, venous ulcers
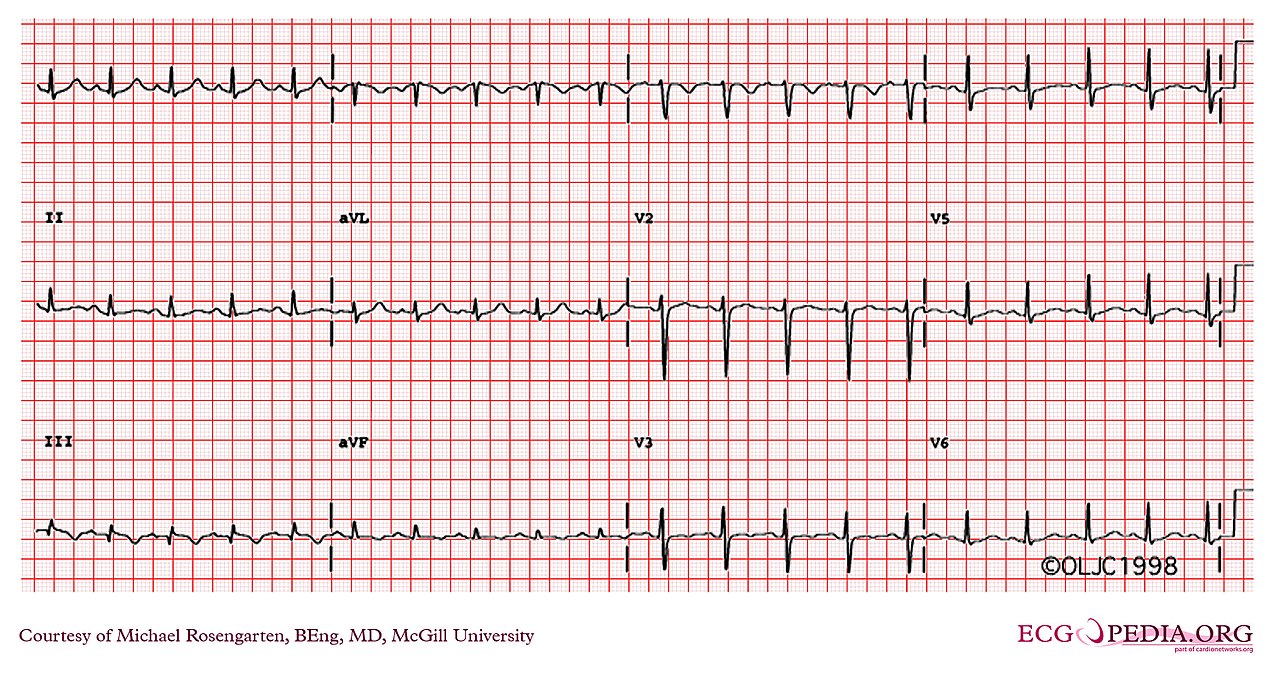
Right bundle branch block due to PE
Wells’ Criteria
DVT and PE risk factors: Previous DVT, active cancer during previous 6 months, immobility for > 3 days
DVT risk factors: Major surgery during previous 3 months
PE risk factors: Previous PE, major surgery during previous month
S1Q3T3
S wave in lead I, Q wave in lead 3, inverted T wave in lead 3
S wave = downward deflection after QRS complex (similar to a Q wave, but after the QRS)
Rarely seen in PE EKGs
Anticoagulation
Should not exceed 3 months if a reversible provoking factor/etiology is identified (see Wells’ criteria above)
Lovenox should be continued in patients with active malignancy
Apixaban
Selected over rivaroxaban in this vignette because rivaroxaban must be taken with food
Apixaban reduce dosing applies to patients who meet two of the following criteria: Age > 80 years, weight < 60 kg, serum creatinine > 1.5
Pt with h/o heart failure, PNA, and malignancy presents with acute on chronic dyspnea. Reports recent surgery with subsequent immobilization lasting > 3 days. ROS positive for fevers/chills, cough/hemoptysis, pleuritic chest pain, myalgias. Fever, tachycardia, tachypnea, JVD, diminished breath sounds, crackles, pleural friction rub, chest wall dullness to percussion, abdominal ascites, hepatosplenomegaly, lymphadenopathy, and LE edema on exam.
Labs
Obtain initial CBC, CMP
Consider obtaining BNP, TSH, urine protein
Obtain serum protein and serum LDH at the same time pleurocentesis is performed (see below) and evaluate etiology per Light’s criteria
Imaging
Obtain PA/lateral CXR
Consider pleural U/S, thoracic CT
Treatment
Effusion due to heart failure: Medical management
Not due to heart failure with effusion > 1 cm on decubitus or > 5 cm on lateral film:
Unilateral effusion: Schedule ultrasound guided thoracentesis and obtain fluid protein, LDH, pH, Gram stain, cytology, and culture. Consider obtaining fluid amylase, cholesterol, triglycerides, tumor marker, and M. tuberculosis culture.
Bilateral effusion: Consider thoracocentesis in setting of fever, pleuritic chest pain, or large effusions
Exudative effusion with unclear etiology or complicating factors: Consult pulmonology
Definition: Fluid collection between parietal and visceral pleural surfaces
Etiology
Transudative (increased hydrostatic pressure or decreased oncotic pressure)
Common: Heart failure
Less common: Cirrhosis, nephrotic syndrome
Rare: Superior vena cava obstruction
Exudative: Inflammation/disruption of pleural lining typically due to primary lung etiologies
Viral/bacterial infection/PNA: Fever/chills, cough, myalgias
Pulmonary embolism: Immobilization, pleuritic chest pain, hemoptysis, tachycardia
Malignancy
Due to cardiothoracic surgery
Effusion is exudative if it meets one of Light’s criteria
Pleural fluid protein / Serum protein > 0.5
Pleural fluid LDH / Serum LDH > 0.6
Pleural fluid LDH > (2/3)*Serum LDH upper limit of normal
Further information: Dx - The Clinical Problem Solvers
Pt with h/o congenital heart disease/failure, OSA, COPD, PE, DVT, systemic sclerosis, HIV, and schistosomiasis presents with dyspnea on exertion and fatigue. Reports recent angina, syncope. SPO2 < 90%, JVD, LE edema on exam.
Obtain CBC, BMP, BNP, TSH
EKG shows R ventricular enlargement, right bundle branch block, and S1Q3T3 pattern suggestive of PE
Echocardiogram indicates pulmonary arterial pressure > 25 mmHg
Refer for pulmonary function testing, sleep apnea testing
Pulmonary arterial pressure > 35 mmHg: Refer to cardiology for possible R heart catheterization
Treatment
Vaccination
Administer influenza vaccine, PPSV23
> 65 y/o: Administer PCV13 followed by PPSV23 in 6 months to 1 year
No h/o COPD: Start nifedipine ER 60 mg daily
Resting SPO2 < 88% and/or PaO2 < 60 mmHg: Start oxygen therapy
Etiology-specific
Optimize HFpEF and obstructive lung disease regimens
Chronic pulmonary thromboembolic disease: Consider lifelong anticoagulation and/or pulmonary endarterectomy
Referral
Condition complicated by heart failure: Refer to cardiology
Refer to pulmonology based on right heart catheterization results
Pt counseled that guidelines advise against pregnancy and recommend long-active reversible contraception
Normal pulmonary artery pressure = 25 mmHg
Potential etiologies
Group 1
Includes congenital conditions, connective tissue disease, iatrogenic
Specific risk factors: HIV, systemic sclerosis, congenital heart disease, and schistosomiasis
Group 2: Chronic heart failure (left heart disease)
Group 3: Obstructive or interstitial lung disease
Vasodilators (e.g. nifedipine, sildenafil, bosentan) create ventilation-perfusion mismatch and can worsen symptoms
Start supplemental oxygen when PaO2 < 60 mmHg
Group 4: Chronic pulmonary thromboemboli (endarterectomy may be indicated)
Group 5: Multifactorial, e.g. sickle cell disease
Most common cause of death is right heart failure