Heart Failure
Elderly patient with history of hypertension, coronary artery disease, valvular heart disease, atrial fibrillation, and diabetes mellitus type 2 presents with dyspnea on exertion, fatigue. Reports new onset orthopnea, nocturnal cough. Heart rate > 120 bpm, jugular venous distention, hepatojugular reflux, bibasilar crackles, S3 gallop, 2+ pitting lower extremity edema on exam.
Patient meets Framingham heart failure diagnostic criteria
Labs
NTpBNP > 400 pg/mL
Obtain CBC, ferritin, TIBC, CMP
Consider lipid profile, TSH, U/A, HbA1c
Imaging
Atrial fibrillation on EKG
CXR shows cardiomegaly, venous congestion, interstitial edema with Kerley B lines
Echocardiogram shows (one of the following patterns):
Preserved ejection fraction: LVEF > 50%, elevated LA pressure, impaired LV relaxation, decreased compliance, and E/A reversal
Reduced ejection: LVEF < 50%
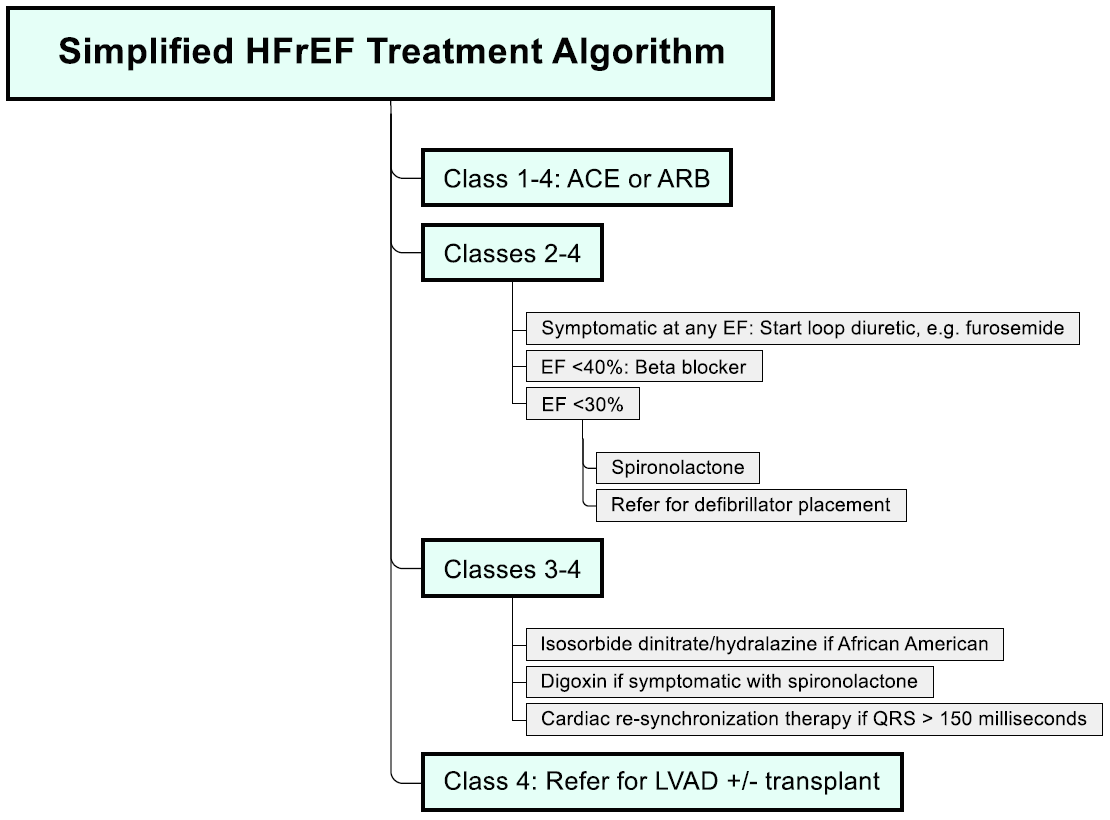
Treatment
Patient counseled about weight loss, dietary sodium reduction, smoking cessation
ACE inhibitor: Lisinopril
Preserved ejection fraction: Start 5 mg daily and increase by 10 mg every two weeks to target dose of 40 mg daily
Reduced ejection fraction: Start 10 mg daily and titrate to 20 mg daily as needed for blood pressure control
Additional medications
EF < 40%: Metoprolol succinate 50 mg daily
Symptomatic (e.g. dyspnea): Chlorthalidone 25 mg daily
Start statin if patient qualifies
Atrial fibrillation at any EF
Aspirin 81 mg + anticoagulation per CHA2DS2-VAsc
Metoprolol succinate 50 mg daily
Heart failure with reduced ejection fraction (HFrEF)
Hypervolemia
Fluid restrict to 1.5 L daily to correct hypervolemia, hyponatremia
Hypervolemia refractory to fluid restriction: Stop chlorthalidone, start bumetanide 1 mg daily and titrate to 2 mg daily
Ferritin < 100 ng/mol
Administer 1000 mg IV iron ferric carboxymaltose bolus
Schedule follow-up at 6, 12, 24, and 36 weeks to monitor anemia
LVEF < 30% with GFR > 30 mL/min
Start spironolactone 12.5 mg daily and double dose every 4 weeks to 50 mg daily while monitoring for hyperkalemia
Persistent symptoms despite spironolactone: Consider digoxin 0.125 mg daily
LVEF < 30% and fatigue, palpitation, dyspnea, or anginal pain provoked by moderate exertion: Consult cardiology for defibrillator placement
Additional considerations
Consider transition of ACE to Entresto (valsartan + sacubitril) in patients with HFrEF class II-III to improve outcomes
African American with uncontrolled HTN on ACE/beta-blocker: Consider isosorbide dinitrate/hydralazine (Bidil) 1 tablet TID
Angina/chest pain present: Obtain stress test (may require catheterization)
Follow up as outpatient within 7 days after hospital discharge to reduce readmission rate
Notes
Non-hypertensive Causes of Heart Failure
Cardiac: Pericardial constriction, primary valvular disease, atrial myxoma
Infiltrative disorders: Amyloidosis, sarcoidosis
Storage disorders: Hemochromatosis
NYHA Stages of Heart Failure
No limitation of physical activity
Light limitation of physical activity: Ordinary activity causes fatigue, palpitations, or dyspnea
Marked limitation: Less than ordinary activity causes fatigue, palpitations, or dyspnea
Unable to engage in physical activity without symptoms, or symptoms that occur at rest
HFpEF
Definition: EF > 50% with s/sx of HF (diagnosis of exclusion)
Pathophysiology
Reduced ventricular compliance reduces ventricular filling during diastole
Most commonly associated with LV hypertrophy
Treatment
Controlling hypertension improves prognosis
Beta-blockers reduce heart rate and improve ventricular filling
HFrEF
Medications that improve mortality
Beta-blockers
Approved agents: Metoprolol succinate, carvedilol (Coreg), bisoprolol
Start in all patients when euvolemic and stable
Contraindications: Hemodynamic instability, bradycardia, severe asthma
Aldosterone antagonists (e.g. eplerenone, spironolactone) in patients with EF < 35% and symptomatic HF (survival advantage observed within 30 days)
Vasodilators: Hydralazine, isosorbide dinitrate
Additional medications
Diuretics and digoxin: Improve symptoms, but do not decrease mortality
Amlodipine may help control blood pressure, but does affect HF outcomes
Verapamil: Negative inotropic effect worsens heart failure
Statins do not improve outcomes for patients who do not otherwise meet criteria for lipid-lowering therapy, see CORONA, GISSI-HF trials
BNP
Volume expansion → increased ventricular pressure → ventricular dysfunction → BNP release
Renally cleared, i.e. ↓ Cr clearance = ↑ BNP
BNP > 400
LR = 19 for heart failure
Does not necessarily indicate acute exacerbation
HF exacerbation: BNP at admission is correlated with inpatient mortality